

There are several assumptions made when a patient presents to the hospital with a fragility hip fracture: a) the fracture will be repaired b) the patient will recover and c) the patient will eventually go home or to rehabilitation. Should they pursue the palliative care route or proceed with surgery? The family is left with an hour to think things over. The family is informed that the risk of not having surgery will likely result in death, yet in this patient’s case, proceeding with surgery carries its own risk. Interprofessional teams (surgery, anesthesia, nursing) are of differing opinions.
Between her cardiac and pulmonary function, the surgery poses an increased risk of perioperative complications-she may never survive the surgery, or come off of the ventilator once she is intubated. Her pre-operative assessment also revealed a heart murmur the resulting echocardiogram demonstrated a heart in very poor condition, with significant valve issues. On admission, the team discovered a pleural effusion, taking up much of her right lung.
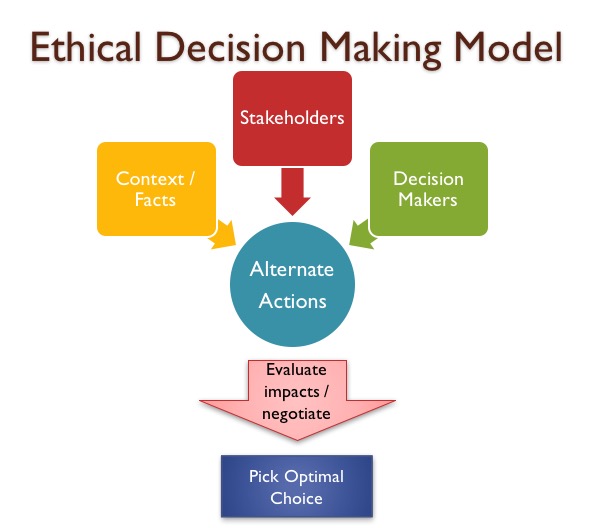
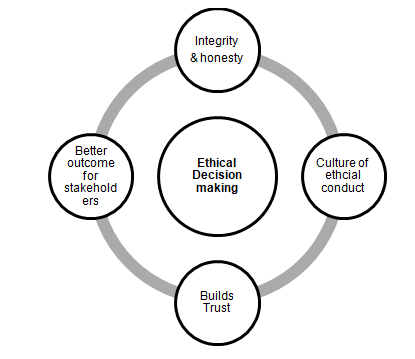
They state her health has been declining over the last few weeks, with increasing confusion and she now rarely leaves her room. She has limited mobility, previously used a walker. Jones has dementia and is unable to make her own decisions. She was admitted to hospital with a fragility hip fracture after being found on the floor in the middle of the night. Jones is 93 years old and lives in a Long Term Care residence. ( 8) 8-step framework (see Appendix A) for ethical decision-making. To better understand the underlying ethical complexities which arise from critical decisions in the acute care setting, this paper will examine a case study to demonstrate application of the Corey et al. ( 4, 5) Patients and families have reported in the past that they feel left out of crucial conversations and decisions surrounding care, ( 6) and that relevant information is not always provided. ( 3) Patient-centred care is “a moral concept and philosophy, considering it to be the right thing to do when designing and delivering respectful, humane, and ethical care”. Unfortunately, as a short pre-operative interval predicts the best outcomes, patients and families face a difficult and hurried decision, potentially with limited time to voice their concerns, and little to no information on which to guide their decision.įrom a systems perspective, quality of care and health outcomes have not always incorporated the patient-centred perspective. The patients at higher risk of poor outcomes perioperatively deserve the opportunity to explore options and articulate their values. ( 1, 2) The majority of patients are good candidates for surgical repair however, given the risks of anesthetic and trauma of the operative procedure, surgery may not be the best choice for all. The Ministry of Health and Long Term Care of Ontario has promoted best practice recommendations which advocate for immediate surgical repair, within 48 hours of admission, in order to achieve optimal recovery outcomes. Is every fragility fracture a candidate for surgery, no matter what the outcome? When is it right to discuss other options with the patient? This article examines a case study via an application of a framework for ethical decision-making.Įvery year, over 30,000 Canadian older adults experience a fragility hip fracture. Similarly, health-care providers may experience moral distress or hesitancy to articulate other options, such as palliative care. Patients and families face a difficult and hurried decision, often with no time to voice their concerns, or with little-to-no information on which to guide their choice. The majority of patients are good candidates for surgical repair however, for some patients, given the risks of anesthetic and trauma of the operative procedure, surgery may not be the best choice. These best practice standards advocate for immediate surgical repair, within 48 hours of admission, in order to achieve optimal recovery outcomes.
In Ontario, the Ministry of Health and Long Term Care has implemented strategies to reduce surgical wait times and improve outcomes in target areas. In Canada, up to 32,000 older adults experience a fragility hip fracture.


 0 kommentar(er)
0 kommentar(er)
